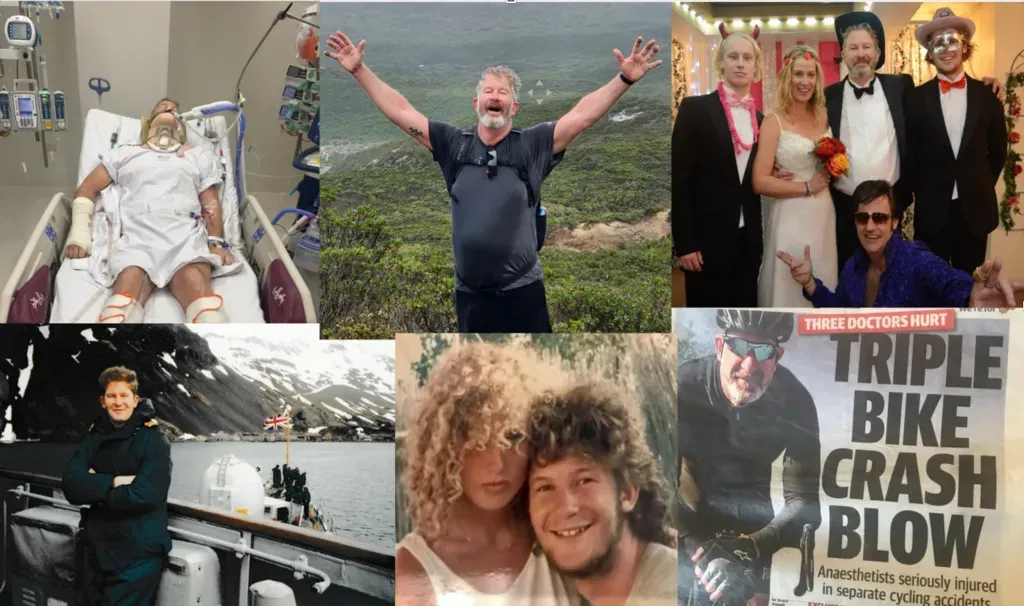
High Performance and Brain Injury
System Overload
High Performance after Brain Injury
When we think about high performance, we picture fast-jet pilots, trauma surgeons, special forces operators performing complex tasks under pressure, lives on the line, alarms sounding, and time fading away. We rarely associate high performance with standing in a supermarket aisle, pondering whether to buy Crunchy Nut Cornflakes or Coco Pops. For many of those living with a brain injury, everyday life is an endlessly demanding, exhausting and even distressing environment, with no applause or medals.
High-performance management is not about brain brilliance; it is about managing cognitive load, preserving bandwidth, and creating systems that reduce our brain’s workload and prevent meltdown. That insight matters in cockpits, frontline operating theatres, and supermarkets alike.
Cognitive Load is the Enemy
Let us start with a straightforward fact that applies to us all. The human brain has a limited working capacity and when that capacity is exceeded, just like a computer running too many programs simultaneously, performance degrades, errors increase, and in the worst case, the system collapses. In addition, with humans, cognitive overload causes fatigue to accelerate, and decision-making processes to become unreliable.
In elite environments, this is treated as a design problem, not a personal failing. High performers do not rely on talent; they engineer simplicity; pilots do not memorise every checklist because they are forgetful; they use checklists because even the elite have working memories that are fragile under stress; trauma teams do not improvise roles during a resuscitation, they assign tasks in advance because ambiguity and uncertainty consume cognition.
Now consider the cognitive reality of someone with a brain injury. Simple conversations are exquisitely complex if you are unable to filter and manage the inputs and outputs. Language, tone, intonation, facial expressions, hand gestures, and body position are complex before we even try to understand what is said, and why. We have not even got to planning a day, filtering noise, remembering instructions, managing fatigue, and regulating emotion. Ask an AI specialist how enormous those tasks would be if they had to write lines of code for each step.
None of these is a subconscious operation anymore. They are front-and-centre with the brain working closer to its limits, more often, with fewer reserves. That is not low performance. That is high load and elite performance, to survive.
Deficit and Disability
Society frames brain injury as a deficit problem.
What can’t you do? What did you forget? Why are you angry? Are you stupid?
If we assume competence, we will ask different questions.
How do we protect high-performance cognition? How might we excel for longer?
This altered perspective matters because a person with a brain injury is not failing to cope with life; they are operating in a permanently narrowed bandwidth environment, like an experienced high-level pilot working amid harsh environments with multiple targets and hunted by aggressive adversaries.
How might we share strategies across the spectrum of cognitive bandwidth?
Reduce the Load Before You Increase the Effort
In high-risk professions, the first response to overload is not to try harder. Fighter pilots reduce tasks during key moments of flight; surgeons standardise procedures to avoid unnecessary variation; emergency services use protocols. All adopt the same strategies, not because they lack intelligence, but because intelligence must not be focused on unavoidable, crucial decisions.
For brain-injured individuals, this principle is transformative. If the day is overwhelming, the solution is not motivation; it is to re-design for fewer decisions, fewer transitions, fewer environments, fewer inputs, fixed routines, binary choices, and predictable schedules.
This is not giving up; this is skilled, elite, load management.
Automaticity is the Goal
Automaticity, executing a task without conscious effort, is the hallmark of elite performance under pressure. Automaticity expends little cognitive energy and is reliable under stress. Elite performers do not perform better because they think more; they perform better because they think less. This principle applies directly to brain injury recovery.
Automaticity is a trained skill; not once, not twice, but repeatedly. Morning routines, medication, transport, communication scripts, and energy management all help reduce the load of a person living with brain injury. If a task requires active thinking, it will eventually fail under fatigue. It is commonplace for rehabilitation to emphasise task completion rather than task efficiency.
The question should not be 'Can you do it?' but 'Can you do it without thinking?'
Externalise Cognition Without Shame
We are reassured when we see a pilot or a doctor working through checklists, recognising that these strategies allow for complex planning and issue resolution. High performers aggressively, obsessively, habitually offload their cognitive burden, routinely employing checklists, whiteboards, stopwatches, standardised language, and call-and-response communication.
External memory aides for routines and checklists are safer than internal memory, yet people living with brain injuries are told to improve their memory. This is the wrong target. The target should be to remember less and thus, calendars, alarms, notes, visual and surrounding prompts are not aids, but cognitive prosthetics. By associating such strategies as those of elite individuals, we remove the social stigma around such survival tactics for those living with brain injury.
Fatigue is not a Sign of Weakness
In elite settings, fatigue is relentlessly monitored because it is dangerous to exceed accepted parameters. Tired people underestimate the impact of cognitive fatigue. Ironically, those with limited cognitive bandwidth become much more aware of their own fallibility and frailty. Ignoring this fact in either group, is not resilience; it is malpractice. Flight hours are regulated, shifts are limited, and mandatory rest is enforced. For those living with a brain injury, lack of self-awareness, reckless behaviour and disinhibition make fatigue a familiar and challenging proposition.
Thus, high-performance and brain injury behaviour means planning rest, scheduling challenging tasks early, protecting recovery time, stopping BEFORE collapse, pacing as good practice, and always being load-aware.
Language Matters
Language is an essential part of rehabilitation for those living with a brain injury. While cognitive loss can be problematic, loss of identity is most common and potentially devastating. When we frame a person living with brain injury as impaired, dependent, or fragile, we strip them of agency. The language of high-performance psychology does the opposite and treats individuals as remarkable operators constantly under demanding conditions. A simple reframing of the language restores dignity, confidence, and further boosts performance.
'You are working at your maximum bandwidth', rather than 'you aren’t coping'.
'You are remarkable' rather than 'you are damaged'.
What This Means for Rehabilitation
Rehabilitation must move beyond skills training and become performance engineering, designing environments that reduce load, training automaticity instead of insight, building routines that survive fatigue, normalising external supports, and respecting limits without judgement. This is not lowering expectations; it is understanding the hurdles of the brain-injury environment, just as we do with our elite performers.
What This Means for Society
If we understood brain injury as a high-performance challenge, we would design work differently. We would design public spaces differently. We would stop equating independence with isolation. We would stop asking people to overcome biology with willpower.
High performance does not work that way.
Conclusion
Dr Stephen Hearns (Peak Performance Under Pressure) writes about excellence under pressure in extreme environments. Still, the most extreme environment many people will ever face is ordinary life with a brain that no longer filters, prioritises, or recovers the way it used to. These individuals are not low performers; they are operating at the edge of capacity every day. The question is not whether they can rise to the challenge; the question is whether we will finally give them the tools that elite performers have learned to use. If we do, something remarkable will happen; performance returns, confidence stabilises, identity rebuilds.
Let us stop pushing harder and work smarter; create resources that respect the limits revealed by high pressure and cognitive load.
Coping with the limiting bandwidth of a brain injury IS high performance.